Summary
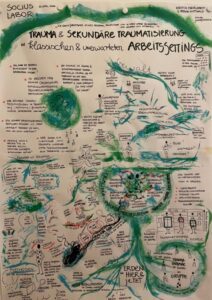
The text deals with the topic of trauma and traumatisation in various work environments. The phenomenon of traumatisation, with its consequences and effects, manifests itself both intra- and interpersonally, as well as in contexts that were previously unprepared or ill-equipped to deal with it. Employees may experience such events as overwhelming and react in different emotional and physical ways. The text first explains the reason for addressing this topic. It then presents the different levels of trauma, the influencing factors and the effects. Finally, it discusses how this can be dealt with in a work context.
The unexpected experience
They cry. They are aggressive – in their attitude, in their language. They are distraught. They want to tell their story, in detail, whether asked or not. They want attention.
The foundation's employees were not prepared for this. They are not trained for it either. They are overwhelmed, sometimes overworked. And they react in different ways: with fear of direct contact; with irritability, frustration, cynicism, exhaustion. Or physical symptoms appear: from tension to sleep disorders. And what remains is the overwhelming feeling of not being able to do justice to the situation and the people involved.
We were invited to attend a training course on the topic of Unsettling places We sat opposite employees of a foundation that deals with a specific historical period after the Second World War. Among other things, it offers a large exhibition on this topic. The employees came from the fields of education, libraries and archives. Almost all of them are in direct contact with visitors on a regular basis. Visitors view the exhibition, use the library or request documents from the archive, often relating to their own (family) history. Others make contact by telephone or digitally.
We spontaneously changed the programme and designed the rest of the training course around the topic of trauma: trauma in its various forms, such as primary, secondary and intergenerational trauma. We also discussed how to deal with traumatised individuals. We then introduced the method. Peer counselling The participants tested the method in smaller groups. In this way, they developed an initial small pool of possible courses of action for the various situations that arise.
Neither the managers nor the employees were prepared for people with symptoms of trauma. Nor were they prepared for what such encounters trigger (or can trigger) in themselves.
They were and are not the only ones. Only recently has the issue of trauma been recognised in professional fields that previously seemed unaffected by it.
As luck would have it, following the above-mentioned training course, we received further commissions from other institutions on the subject of trauma and its consequences. We conducted a large internal survey among dozens of doctoral students whose research topics also included violence – both in historical and contemporary research topics. And we conducted further training courses for institutions whose employees were also unprepared to deal with trauma.
Before we present some basic information on the subject of trauma and traumatisation below, here is a note: the term „traumatised“ has become a frequently used term in everyday language. It is often used to describe annoying or bothersome experiences. For example: „I'm gradually becoming traumatised; the train was late again.“ The clinical term differs fundamentally from this.
Basics on the topic of trauma
The German Trauma Foundation defines trauma as „a stressful event or situation that the person affected is unable to cope with and process. It is often the result of violence – both physical and psychological. It can be described figuratively as a „mental injury“.“ What is described here is Primary traumatisation. The adjective „traumatised“ refers to this psychological connection.
The clinical classification system ICD-10 Formulated as a trauma criterion:
„[…] a stressful event or situation of shorter or longer duration, involving exceptional threat or catastrophic proportions, which would cause profound distress in almost anyone (ICD-10) (e.g. natural disaster or serious man-made calamity – man-made disaster – combat operations, serious accidents, witnessing the violent death of others or being a victim of torture, terrorism, rape, abuse or other crimes). And further:
This event
- causes extreme stress, feelings of horror, helplessness and loss of control; both when someone is affected by the event themselves and when they witness other people becoming victims of such an event
- causes a violation of personal boundaries and a loss of trust in fellow human beings, technology or the environment
trauma
The term „trauma“ comes from ancient Greek. trauma: wound/ Injury. In plural: „Traumas“, “Traumas“.
ICD 10
International Classification System of Diseases. The ICD-10 is the 10th revision of the International Statistical Classification of Diseases and Related Health Problems the World Health Organisation (WHO). It is used to encode medical diagnoses. (On 1 January 2022, the ICD-11 with further disease diagnoses. After a transition period of at least 5 years, the coding only according to ICD-11).
- Finally, due to the brain being literally flooded by such an overwhelming stress reaction, it is unable to process the experience appropriately; the experience cannot be integrated into the treasure trove of experiences as usual, and it is not possible to gain distance from it. This overload of the innate biological stress system has psychological and possibly also physical consequences.
To get from a Trauma in the clinical sense To assume this, the following three criteria must be met:
- The event poses an existential threat and would be perceived by most people as a serious threat.
- Those affected are overwhelmed by processing what they have experienced and have exhausted their personal resources.
- The event has a lasting impact on those affected, resulting in suffering and impairment in coping with everyday life.
However, not every stressful experience causes trauma in those affected. More on this below.
The phenomenon of trauma can be summarised as follows:
- Psychological trauma can affect anyone
- it is an extremely threatening event
- it exceeds our ability to cope
- A person can experience the event (1) as a victim, (2) as a witness, or (3) indirectly (e.g. through visual or written reports of disturbing events or confrontation with trauma-related stimuli in the course of their professional activities).
- the event causes strong unpleasant emotions such as fear, helplessness, powerlessness
- the event would plunge pretty much anyone else into despair as well
- the event has a lasting impact on one's understanding of oneself and the world
- Traumas can be classified according to frequency or cause.
- Traumas can be divided into
- Shock trauma: a single, isolated event that is usually well remembered.
- Developmental trauma: usually high levels of stress over a prolonged period; often associated with feeling unsafe anywhere.
- Social trauma: an event that affects many people (e.g. train accident)
- Trauma reactivation in old age (see below)
- transgenerational trauma (see below)
- Secondary trauma or indirect trauma (see below).
PTSD
The Post-traumatic stress disorder (PTSD) occurs as a delayed psychological reaction. Typical symptoms of PTSD are the so-called symptoms of reliving the experience, which affect sufferers during the day in the form of memories of the trauma, daydreams or flashbacks, and at night in the form of nightmares. PTSD sometimes only occurs after a long period of time.
The following are considered symptoms and consequences of trauma:
- Hypervigilance (constant overexcitement): high tension, insomnia, eating to calm down, substance abuse (addiction), inner restlessness, anxiety and panic states, panic attacks, difficulty concentrating, tantrums, hyperactivity, erratic behaviour
- Flashbacks (memories that catch up with people as if they were experiencing the situation again)
- Obsessive-compulsive disorder, depression, anxiety disorders
- In cases of under-stimulation: exhaustion, lack of energy, listlessness, disturbed eating habits, substance abuse (addiction), feelings of meaninglessness, isolation, feeling different and alienated.
- However, more subtle, less obvious symptoms also occur very frequently.
Traumas can be viewed in context:
- Traumas experienced as a group are easier to overcome than those where you feel that it happened „only to me“.
- A traumatic event is also easier to cope with in the case of fateful events or random disasters, e.g. natural disasters.
- It is much more difficult when the trauma is caused by another person – perhaps even someone close to you or someone you trust („man-made trauma“).
- Permanent trauma, i.e. repeated or prolonged exposure, leads to post-traumatic stress disorder (PTSD) more often than a single experience.
- The effects also depend on personal factors (social network, general mental state, age, pre-existing conditions, resources).
- In many cases, acute stress reactions disappear just a few weeks after a single event, without the affected person having to do much about it. Often, a safe environment is enough for the psyche/soul and the organism to find peace and for the person concerned to regain control over their own life.
Past traumas can be reactivated in old age:
Often, people are able to lead a more or less normal life even after a trauma, thanks to their available resources and the tasks they are faced with. Their coping strategies are sufficient to deal with the stress. Caring for their own children, looking after relatives or professional commitments mean that their focus is directed towards other important areas of life; as a result, the trauma recedes into the background for a time, sometimes for years.
However, with increasing age, resources (coping mechanisms) decline, e.g. due to further infirmities, illnesses or other stresses. If a critical threshold is exceeded, the coping mechanisms may no longer be sufficient. Then, trauma memories suddenly become very present for those affected and trauma-related disorders can develop, including health symptoms or social problems. Then, even everyday signals – smells, noises, certain situations – can reactivate the fears of the past (triggers) and overwhelm the person affected. This is when the trauma is reactivated. And sometimes it happens without there being a specific memory of the event that caused it.
This reactivation mainly affects people aged 65 and over.
Another level of trauma is transgenerational trauma transmission:
Epigenetics provides important insights here. Epigenetics deals with the interaction between environment and genetics. According to this, external factors can influence genes and also switch them on and off. This is how ancestors pass on their experiences to their descendants via their altered genes. The descendants carry fears, self-doubt or shame within them, for example, without understanding the reasons or connections.
This does not mean that trauma-related disorders are predetermined in offspring (every person has two parents), but there may be a certain vulnerability.
Sexualised violence
Sexualised experiences of violence often cause double suffering: the subject of sexual violence was hushed up at the time and is still a source of shame for those affected today – this can make it extremely difficult to process or deal with the trauma.
PTSD in old age
Post-traumatic stress disorder (PTSD) is found at above-average rates in older patients.
Secondary traumatisation
Furthermore, there is secondary traumatisation, also known as „indirect“ traumatisation:
Secondary traumatisation describes traumatisation that occurs without direct personal experience of the original trauma. It can develop through frequent or regular contact with traumatised individuals and/or their relatives. Or it can arise from frequent or recurring exposure to visual, auditory or written accounts of stressful events such as violent crimes, natural disasters or wars. Those affected show symptoms similar to those of people with primary traumatisation. Secondary traumatisation usually develops gradually.
Secondary traumatisation usually occurs in a professional context. According to current research, occupational groups such as psychotherapists, supervisors and, for example, police officers are affected, as well as members of helping professions in general, such as firefighters, emergency responders, social workers and nurses. But archivists, journalists and scientists can also be affected. Historians, for example, spend years dealing with the same horrific crimes, talking extensively to witnesses and processing unvarnished image and audio material. Or archivists record documents relating to criminal trials involving acts of violence of all kinds. (See also: https://intrapsychisch.de/sekundaere-traumatisierung)
Why some people develop secondary traumatisation in a professional context and others do not depends not only on the professional task situation, but also on the individual person and their life circumstances.
People with secondary traumatisation usually have a compassionate attitude: their brain produces an emotional response to the described or documented event. The same stress hormones are released as in people who experience the trauma directly.
Other factors that play a role include resilience or existing or insufficient coping strategies, the respective situational context, the social environment and the person's own traumatic experiences. Finally, depictions of violence perpetrated by humans against humans (man-made trauma/man-made disaster) tend to be more disturbing than, for example, natural disasters.
However, the greatest risk factor is persistent preoccupation with traumatic content, whereby this traumatic content can vary.
Friedrich Nietzsche put it this way: „If you gaze long into an abyss, the abyss also gazes into you.“
Trauma-sensitive in the work context
Currently, trauma-sensitive interaction with one another in the workplace is being discussed and, in some cases, implemented. Specifically, this means, „Even without knowledge of another person's possible trauma, working in a trauma-conscious manner, alleviating trauma and avoiding retraumatisation, and treating all individuals, with or without traumatic experiences, in a manner that encourages cooperation and dialogue, accompanying them.“.
It is important to avoid making hasty attributions such as „she is traumatised„ and immediately deriving a course of action from this, even if a person shows symptoms that may indicate trauma. In a laboratory conducted by SOCIUS in spring 2024, the following questions proved helpful in sharpening one's own (course of action) perspective:
- Is this an actual diagnosis or my personal assessment?
- What is the specific group, team or organisational context?
- What is my task here?
- Is this, in my micro-context, the right place/the right setting for me to intervene?
- And what can I actually hold, or am I really competent here?
Possible personal reactions or interventions can also be reflected upon in internal or external counselling sessions. Internally, this can take the form of confidential discussions with colleagues, superiors, HR managers and, if available, health officers; or with the help of equally confidential tools such as peer counselling and supervision. However, I can also seek external counselling, e.g. from crisis services such as the Berlin Crisis Service or the telephone counselling. In this way, I take action and assume responsibility while providing the greatest possible protection for the person concerned and myself. And the latter is also important, after all.